Understanding the patient journey has become crucial for improving treatment outcomes and addressing unmet needs. Pharmaceutical companies need deeper insights into the patient experience — from initial symptoms through diagnosis, treatment, and long-term management – to improve market visibility and marketing opportunities, demonstrate the value of treatments and treatment effectiveness, and ensure the right patients receive the right care at the right time.
However, traditional methods of mapping this journey often fall short due to limited data availability, issues with data linkages, and reliance on the data points captured in standard clinical practice, which often do not fully represent the intricacies and diversity of patient experiences.
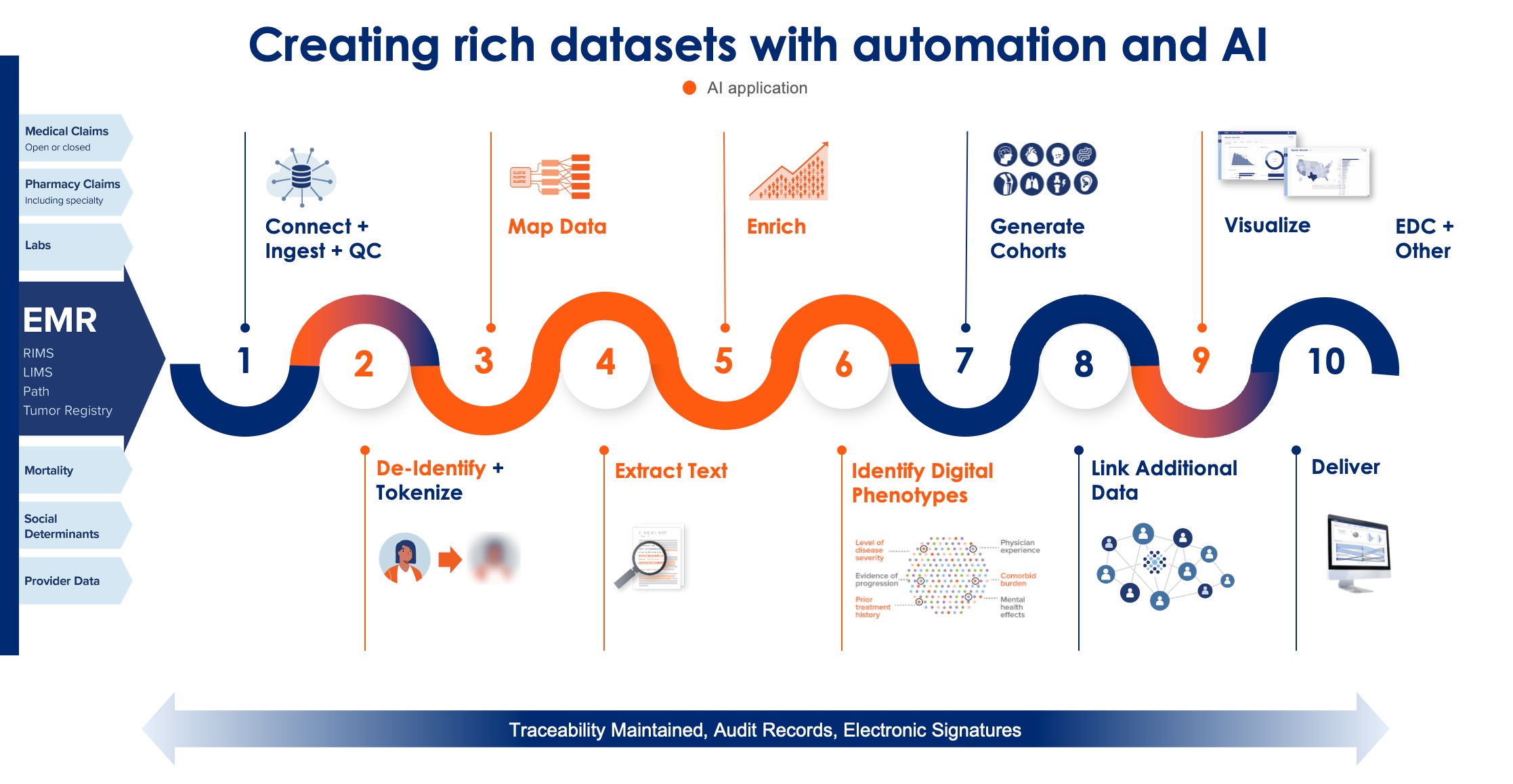
AI-based digital phenotyping technology was developed to meet these challenges. Unlike current methods of patient journey analysis, which are limited by researchers’ ability to pre-specify criteria and hypotheses, digital phenotyping uses large-scale, real-world data—including electronic health records (EHRs), claims, and other patient data—to uncover hidden patterns, identify subgroups, and generate new insights into disease progression, patient outcomes, and treatment responses. These insights offer a more comprehensive and nuanced view of the patient journey than is available using more traditional tools alone.
Defining the Patient Journey
The patient journey describes the sequence of events a patient experiences, starting from the onset of symptoms, through diagnosis, treatment, and ongoing management. While this concept is simple, the reality of each patient’s journey is quite complex. This is especially true in cases of chronic disease because of the multifaceted, often heterogeneous nature and long-term progression timeline of chronic conditions. Patients with rare diseases can also have quite complex journeys, which are especially difficult to capture due to the general lack of data on these patients’ experiences. Traditional approaches to understanding these journeys often involve small, disjointed datasets, and small sample-size clinician interviews. These resources can miss critical nuances and differences in patient experiences, including outcomes, side effects, comorbidities, and the overall drivers around how and why treatment decisions are made. Patient journeys drawn from small datasets where all parameters are ‘visible’ are vulnerable to overgeneralization of the most common or obvious patterns, with subtler signals missed.
Patient Journey Phases

The Challenge of Incomplete Patient Journeys
One of the key challenges in mapping patient journeys is the incompleteness of the data used and available. Traditional methods often rely on limited datasets that may not capture the full spectrum of patient experiences, leading to gaps in understanding. For instance, these methods may not account for variations in patient or provider behaviors, or the presence of comorbidities that significantly affect the course of the disease – claims data are particularly vulnerable to this latter concern. This incomplete picture can make understanding unmet needs or optimizing treatment strategies more difficult. Another challenge is the tendency to view patient journeys as linear and sequential. This approach, while logical, can oversimplify the real-world complexity of patient experiences. In reality, many patients do not follow a straight path from symptoms to diagnosis and treatment. They may experience recurring symptoms, misdiagnoses, or treatment failures, which are not adequately captured in traditional journey maps – especially those summarized through clinical experience, which can tend to ‘narrativize’ and simplify messy real-world patterns. Reliance on linearity can obscure critical insights into patient behavior and treatment outcomes.
Addressing Gaps with AI Phenotyping
AI-powered digital phenotyping offers a powerful solution to these challenges by leveraging large-scale, real-world data to identify patterns in existing patient journeys and provide additional insights into these patients. The process starts with cohorts of patients with characteristics of interest – those diagnosed with a particular disease, for example, or who all respond well to a specific medication. Digital phenotyping uses AI to identify common patterns associated with these characteristics in longitudinal data and then labels others with those same patterns. This approach uncovers subtle signals in patient data that might be missed by traditional methods and broadens visibility into which patients are best characterized by which signals.
Discover hidden patient phenotypic signatures to highlight patients of interest
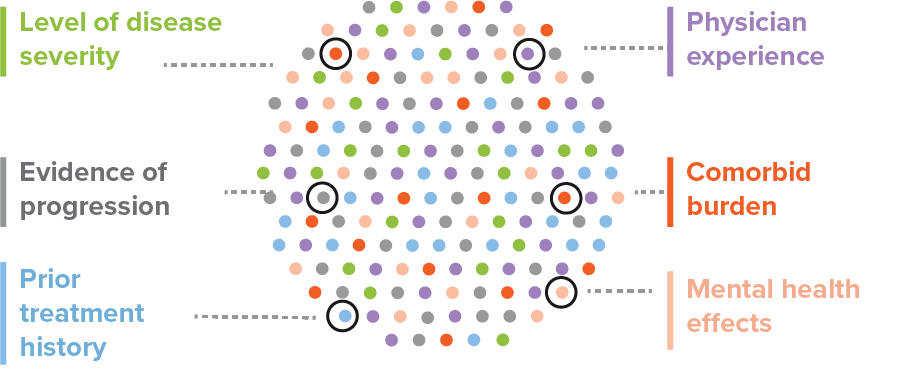
For example, AI phenotyping can help identify undiagnosed or misdiagnosed patients by comparing their health records to those of diagnosed patients with similar characteristics. By recognizing these patterns, pharmaceutical companies can better understand the true prevalence of a condition, the barriers to accurate diagnosis, and opportunities for improving outreach and access to needed treatment. Insights can be added to datasets to improve research into these populations and used to identify practice settings in which patients at greatest risk of undiagnosed disease may be found.
See the complete Patient Journey
Enhancing Treatment Insights
In addition to improving diagnosis, digital phenotyping can provide valuable insights into treatment response. By analyzing patient data before, during, and after treatment, AI tools can identify factors that influence treatment success or failure. This could include understanding why certain patients persist with medication while others discontinue it, identifying the reasons behind adverse events or suboptimal outcomes, and clarifying provider treatment patterns.
These insights are significant for optimizing treatment strategies and developing more effective therapies. For example, by identifying patient subgroups that respond particularly well to a specific treatment, organizations can target these populations more effectively, leading to better outcomes and more efficient use of resources.
Real-world Impact of AI Phenotyping
To illustrate the power of AI phenotyping, consider a few case studies. In one example, OM1 Orion, a digital phenotyping tool designed to enhance the understanding of patient outcomes in datasets, was used to study a subgroup of patients with metabolic dysfunction-associated steatohepatitis (MASH) at high risk of rapid disease progression. By analyzing their longitudinal health records, researchers identified common features in these patients’ data associated with an elevated risk of this rapid progression, allowing for earlier intervention and improved disease management.
In another case, OM1 Orion was used to identify patients more and less to experience negative outcomes following certain treatments for peripheral artery disease (PAD). By recognizing patterns in their health histories, researchers could identify which patients were greatest at risk to improve treatment optimization.
The Future of Patient Journeys
AI phenotyping significantly advances understanding and enhances visibility into patient journeys. OM1’s Orion provides a comprehensive view of disease progression and burden for your patient populations. By filling in the gaps left by traditional methods targeted towards groups and research questions of interest, Orion offers a more complete and accurate picture of the patient experience to enable better-targeted therapies, improved patient outcomes, and more efficient use of resources.
Orion AI insights can augment traditional datasets


As the healthcare industry continues to embrace AI and digital technologies, the potential for improving patient care through enhanced understanding of the patient journey will only grow.
Learn more on how Orion can fill the gaps in your patient journeys:
- Download the eBook
- Secure an AI workshop for your organization with OM1’s Head of AI, Dr. Joseph Zabinski
