 By OM1 | July 16, 2024
By OM1 | July 16, 2024
When dealing with depression research, accurate real-world data is crucial to demonstrate real-world effectiveness. But what happens when critical data is buried in unstructured clinical notes? And how can we leverage real-world data sources for outcomes research when less than a third of all psychiatry and mental health practices use measurement-based care? This post explores how generating estimated PHQ-9 scores from unstructured EHR data with AI can advance depression treatment and research.
The significance of improving mental health outcomes has become undeniably clear over the past few decades. Debilitating mental health conditions like major depressive disorder (MDD) affect millions, worsen other chronic health conditions, and are among the most costly in the U.S., with expenditures surpassing $200 billion per year.1
In this context, the role of real-world data (RWD) in understanding and addressing mental health conditions has never been more critical, with high-quality research-grade RWD essential to drive the discovery, development, and commercialization of new and existing treatments.
The Role of the PHQ-9 in Depression
The Patient Health Questionnaire (PHQ-9) is a validated instrument for screening and tracking the severity of depression. It consists of nine questions that help gauge the presence and intensity of relevant symptoms. Consistently capturing the PHQ-9 over time is important for monitoring changes, understanding response to treatment, and tracking outcomes such as remission and relapse.
Structured Data: The Tip of the Iceberg
While PHQ-9 scores are commonly used, they are not always used or recorded consistently in electronic health records (EHR), complicating the longitudinal tracking of patient outcomes. In the real world, there is often a significant amount of missing data. Coded and recorded disease activity metrics often represent just the visible “tip of the iceberg” in EHR data — and while the PHQ-9 is not always recorded, there is a wealth of critical data regarding symptom severity in depression often found in the structured and unstructured clinical notes that could be leveraged with advanced AI and data science techniques.
By leveraging AI to extract relevant information from deeper layers of clinical data, we can exponentially improve the availability of depression symptom severity measures, thereby enhancing both research and clinical care with better-informed treatment plans and more accurate research findings.
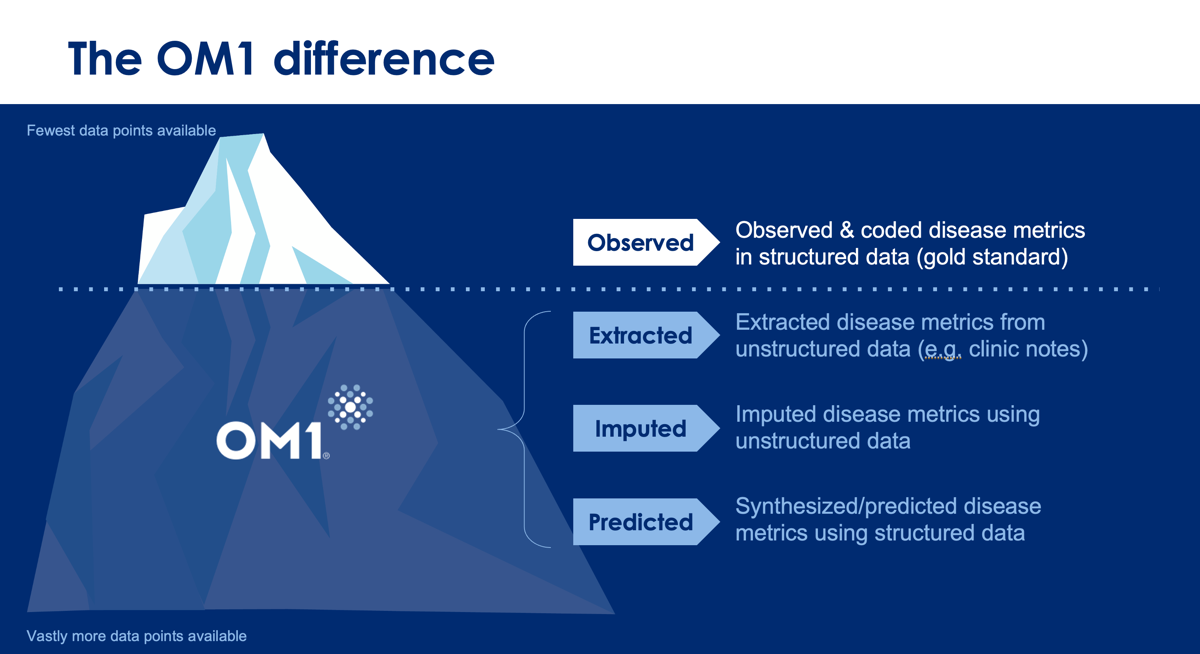
An estimated 80% of medical data remains unstructured and untapped after it is created.2 If we can use these data to estimate disease activity, we can fill in gaps and better understand the longitudinal patient journey – without needing to gather additional data.
Generating Estimated PHQ-9 (ePHQ-9) Scores with AI
In OM1’s AI-powered process, powerful algorithms are calibrated using millions of data points and trained on gold-standard inputs. Our patented machine learning platform is designed to extract and estimate PHQ-9 scores from the OM1 Real-World Data Cloud, a continuously updated, representative dataset of over 340 million U.S. patients derived from deterministically linked, de-identified EHR and claims data from 2013 to the present day.
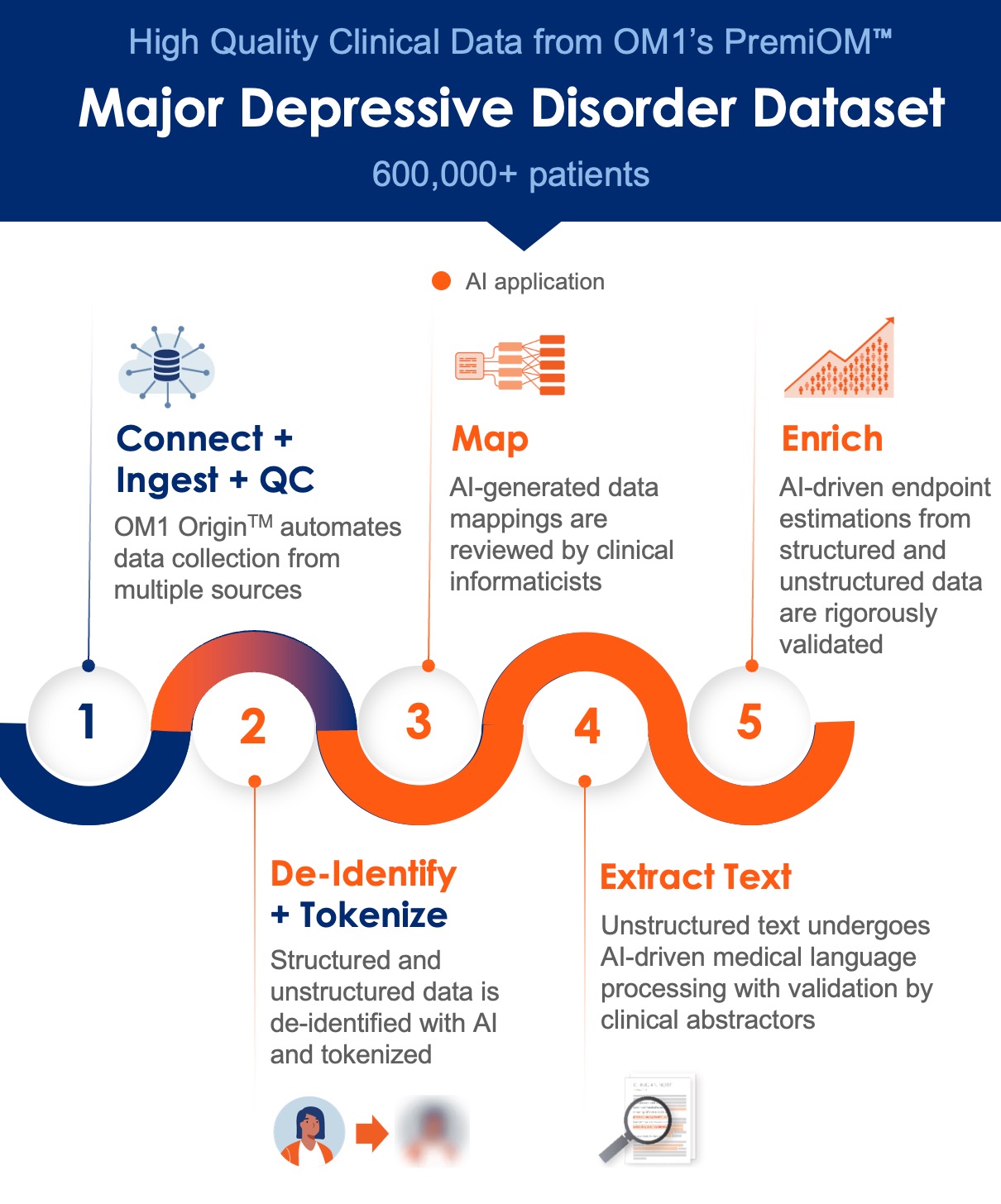
OM1’s algorithms identify collections of linguistic patterns used to document depression severity and associate them with observed PHQ-9 scores on a large training dataset. We then apply those patterns to generate estimated PHQ-9 (ePHQ-9) scores. As part of the validation process, subject matter experts review the clusters of features and organize them into clinically meaningful categories to ensure reliability and explainability. Model performance is evaluated using common data science benchmarks, such as assessment of the area under the curve (AUC), and by calculating the Spearman and Pearson R values typical in developing validated estimated endpoints in other medical specialties.
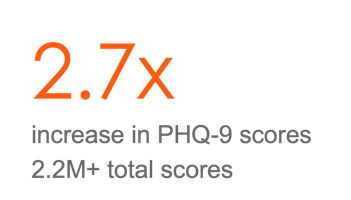
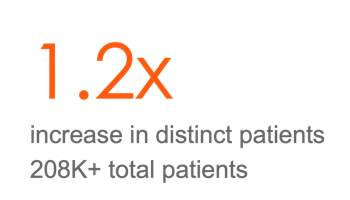
In an OM1 research study presented in 2023, at the American Society of Clinical Psychopharmacology (ASCP), we showed that the application of our model to the OM1 Major Depressive Disorder PremiOM dataset resulted in the generation of new ePHQ-9 scores for more than 2.2 million patient encounters — an increase of 2.7 times over the nearly 800,000 recorded PHQ-9 scores. These estimated endpoints performed well under rigorous evaluation in research with top pharmaceutical companies and can be considered for use in outcome studies alongside the ‘gold standard’ reported patient scores.
Empowering Breakthroughs in Depression Research
The patient journey in depression is often complex and nuanced. By incorporating ePHQ-9 scores, life sciences researchers can gain clearer insights into depression disease trajectories and develop a more comprehensive understanding of the patient journey.
Moreover, expanding the number of patients for whom data points are available not only yields meaningful insights but also establishes a stronger analytical foundation. Research studies conducted with small patient cohorts may overlook significant patterns. Access to larger and more representative patient cohorts not only increases statistical power but also allows for deeper analysis of specific subgroups and the application of more robust inclusion and exclusion criteria in studies.
The use of AI offers a tremendous opportunity to accelerate the clinical development process for mental health conditions and begins to help answer the call for better and faster research into treatments. With the new ePHQ-9 scores and our extensive MDD dataset, we can gain insight into patient populations before, during, and after trials are completed and develop tools to support decision intelligence at the point of care.
About OM1’s Impact on Real-World Data and Mental Health
OM1 is pioneering cutting-edge healthcare innovation through our insights-driven AI technology and data. As the leader in personalized medicine, evidence generation, and real-world evidence (RWE), OM1 has been focused on setting the standard for real-world data outcomes and research in mental health.
OM1’s diverse team of scientists, engineers, researchers, and clinicians with over 30 years of experience in RWD/RWE have led foundational publications such as the Outcome Measures Framework. With support from the Agency for Healthcare Research and Quality (AHRQ) and in collaboration with the National Library of Medicine and the FDA, OM1 led a multi-stakeholder, consensus-based effort to create a harmonized set of depression outcome measures for use in routine clinical practice and research in the mental health and primary care settings.
OM1’s awarding-winning publications in mental health and neuroscience span critical research areas, including:
- Identification of treatment-resistant depression with AI (read more)
- Understanding the side effects of antidepressants and reasons for discontinuation of antidepressants (read more)
- Extraction of suicidal ideation data from clinical notes (read more)
- Evaluating the association of social determinants of health (SDOH) and depression treatment (read more)
Explore the latest research publications in mental health from OM1 »
About OM1 Specialized Depression & Mental Health Real-World Data
OM1’s mental health RWD network includes over 9,000 mental health specialists caring for more than 3.7 million patients, followed longitudinally in over 2,000 clinics in all 50 states. Our specialized datasets in mental health include depression, schizophrenia, bipolar disorder, and more.
PremiOM™ Major Depressive Disorder (MDD) Dataset


Specialty MDD Data

Contact us to discover how OM1’s AI-driven evidence and real-world data in mental health can supercharge your research goals.
Sources:
1https://www.whitehouse.gov/cea/written-materials/2022/05/31/reducing-the-economic-burden-of-unmet-mental-health-needs/
2https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6372467/#B2
